
We just completed the ice storm of 2023 in Texas. Where everything shuts down and I get a bit more time to write a blog.
It's basketball season! I still see quite a bit of ACL injuries. I wanted to write an update on ACL injuries with current literature.
I get a lot of questions about ACLs. When can I return to play? Is it painful? Do I need to wear a brace afterwards? How much physical therapy do I need? What graft do you recommend?
The truth is - there's a lot of differences of opinions in the Orthopedic Community regarding ACL reconstruction in athletes. You can see 5 different surgeons and get 5 different opinions. This does not necessarily mean they are all wrong. There are lots of great surgeons that have successful ACL reconstructions using different techniques. However, I have put together some general guidelines and my personal recommendations based on current literature and evidence based medicine. So here are the top 5 topics and reccomendations, I'd like to give patients.

You tore your ACL (anterior cruciate ligament) and are a young athlete (high school, college, NFL, etc) - now WHAT?
The overwhelming recommendation would be an ACL reconstruction in a young athlete that wants to continue trying to compete at a high level and does a significant amount pivoting to help stabilize the knee. When indicated, ACL reconstruction should be done early as the risk of additional cartilage and meniscal injury starts to increase within 3 months.
1 - PREHAB
There was a recent systematic review that discussed the role of prehabilitation prior to ACL reconstruction surgery. The goals are to increase knee range of motion to baseline and improve quadriceps strength. The length of timing of this in controversial. I recommend 2-4 weeks until patients can get back to full extension and flexion of the knee prior to scheduling a surgery.
This has been found to improve quadriceps strength and single leg hop scores 3 months after ACL reconstruction.
There is no consensus for optimum prehab content, frequency or length.
2- GRAFT CHOICE?
There are two main types of grafts:
- Allograft - harvested from cadaver tissue.
- Autograft - harvested fresh from the patient's own tissue at the time of surgery.
Autografts remain the preferred graft choice in the young athletic patient population due to higher rates of failure, increased costs, and higher risks of rerupture associated with allograft reconstruction. Autograft options include:
- Hamstring
- Patellar tendon and bone
- Quadriceps tendon (with or without bone)
All of these can be harvested from the same knee that was injured or from the contralateral knee. There are advantages and disadvantages of all graft choices, which your surgeon can discuss in detail.
There is controversy in the literature about which autografts have the highest load to failure and stiffness with quadriceps and patellar tendon bone being the top two in most studies. Some have found higher load to failure in quadriceps and some in the patellar tendon groups.
In my practice, I prefer the quadriceps tendon autograft without bone.
3 - PHYSICAL THERAPY
YES. Just yes. You must put in a lot of work with physical therapy to get back to play. Accelerated therapy focuses on improving range of motion on the knee and strengthening of the quadriceps muscle starting immediately after surgery. There is controversial evidence for accelerated therapy vs conventional therapy of restriction from full weight bearing after surgery with no consensus.
I recommend accelerated therapy in my patients. Supervised physical therapy with a licensed physical therapist is more effective than unsupervised physical therapy.
Most patients will be weight bearing as tolerated on the extremity after surgery, but this can change if you have other procedures such as meniscal repairs or cartilage procedures done simultaneously.
There are other modalities, such as Blood Flow Restriction therapy, which has been shown to be beneficial with low-intensity exercise and leads to significantly lower knee joint pain.
Cryotherapy can be beneficial preoperatively and postoperatively as an analgesic (pain control) for patients undergoing ACL reconstruction.
Please contact your surgeon to discuss physical therapy protocols after surgery.
4 - RETURN TO PLAY?
This might be one of the most controversial issues after ACL reconstruction. Historically, patients were returning to sport around 6 months post operatively. Most surgeons have now delayed this to 7-12 months postoperatively due to increasing literature on ACL rehabilitation and reinjury rates.
Most results support the following prior to returning the athlete to sport:
- Importance of psychological readiness in return to sport
- Utilization of FUNCTIONAL and objective testing results
- Development of a secondary injury prevention program
- Having athletes refrain from participating in sports without limitations until at least 9 MONTHS after ACL reconstruction.
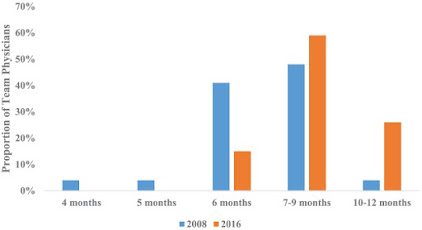
The above graph reports the return to play timeframe for NFL athletes treated by their orthopedic surgeon team physicians. There are 32 total orthopedic surgeons as team physicians in the NFL. You can see that in 2008, it was common for return to play at around 6 months (49%). In 2016 this has shifted to 7-9 and 10-12 months with very few allowing return to play at 6 months (14%).
In my practice, patients will undergo isokinetic testing at 6 and 9 months to evaluate progress and strength in the operative extremity compared to the contralateral extremity and will be re-evaluated for possible return to play at 9 months at the earliest.
5 - BRACING?
The use of a knee brace as part of postoperative protocol has not been shown to provide substantial clinical benefit to patients beyond a psychological sense of security.
Bracing does NOT improve surgical outcomes such as
- limb asymmetry
- Anteroposterior knee laxity (instability)
- Knee joint effusion (swelling)
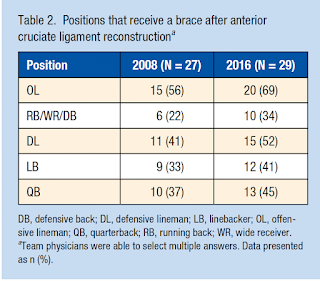
In the NFL patient population, the use of a functional brace after an isolated ACL reconstruction stayed relatively similar from 2008 to 2016 and the majority of team physicians only use bracing for offensive lineman and defensive linemen. 41% of team physicians used the brace for less than 6 months in 2016.
Perhaps the most important question I get from patients and their families is "Will I get to play again?"
I like to discuss the published results from NFL athletes for this. As you can assume, they are the most high level athletes when it comes to football and they are paid to play and have an entire team to help them reach their goals. They train multiple hours daily to be able to return to play. Even with the best trainers, surgeons, equipment for their use, the truth is that the return to play after primary ACL reconstruction was 73%. Factors predictive of successful return to play was:
- Age < 25 years
- High draft picks
- Offensive players
These players played more seasons after ACL reconstruction.
The rate of retear was 4.3% in these patients and 8.5% tear rate of the opposite (contralateral) knee.
In Summary,
If you are a young athlete with and ACL tear, factors associated with better outcomes are prehabilitation prior to surgery, autograft ACL graft and formal physical therapy with 9 months of hardwork.
Now time to focus on the superbowl!
What team are you cheering for?

Resources:
- Carter H, Littlewood C, Webster KE, Smith BE. The effectiveness of preoperative rehabilitation programmes on postoperative outcomes following anterior cruciate ligament (ACL) reconstruction: a systematic review. Orthop J Sports Med. 2020 Sep 30;8(9 suppl7):2325967120S00520. doi: 10.1177/2325967120S00520. PMCID: PMC7543196.
- Buerba, Rafael A. MD, MHS; Boden, Stephanie A. MD; Lesniak, Bryson MD. Graft Selection in Contemporary Anterior Cruciate Ligament Reconstruction. JAAOS: Global Research and Reviews 5(10):e21.00230, October 2021. | DOI: 10.5435/JAAOSGlobal-D-21-00230
- Glattke KE, Tummala SV, Chhabra A. Anterior Cruciate Ligament Reconstruction Recovery and Rehabilitation: A Systematic Review. J Bone Joint Surg Am. 2022 Apr 20;104(8):739-754. doi: 10.2106/JBJS.21.00688. Epub 2021 Dec 21. PMID: 34932514.
- Khair M, Riboh J, Solis J, Maurer J, Brown JB, Vandermeer RD, Cooper DE. Return to Play Following Isolated and Combined Anterior Cruciate Ligament Reconstruction: 25+ Years of Experience Treating National Football League Athletes. Orthop J Sports Med. 2020 Oct 22;8(10):2325967120959004. doi: 10.1177/2325967120959004. PMID: 33150190; PMCID: PMC7585987.
- Brophy, Robert H. MD, FAAOS; Lowry, Kent Jason MD, FAAOS. Academy of Orthopaedic Surgeons Clinical Practice Guideline Summary: Management of Anterior Cruciate Ligament Injuries. Journal of the American Academy of Orthopaedic Surgeons ():10.5435/JAAOS-D-22-01020, January 18, 2023. | DOI: 10.5435/JAAOS-D-22-01020
Source: jillmcangusmd.blogspot.com







